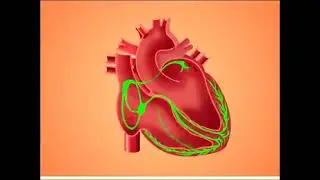
Cardiac action Potential and Effects of Antiarrthymic Drugs
Myocardial action potential and action of antiarrhythmic drugs
CLASSIFICATION OF ANTIARRHYTHMIC DRUGS —
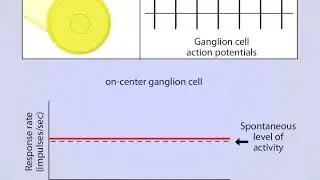
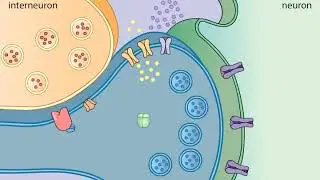
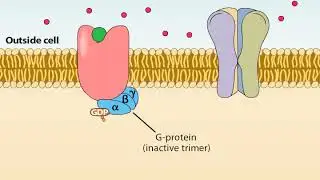
The different antiarrhythmic drugs often have several effects on action potential generation and propagation and may also affect the autonomic nervous system. Those drugs that act on ion channels may preferentially bind to the activated (open) or inactivated state . The classification of antiarrhythmic drugs according to the Harrison modification of the Vaughan-Williams classification was originally based upon their effects on the action potential and also assumes that individual drugs have a predominant mechanism of action . This distinction remains clinically useful even though it does not account for complicated electrophysiologic and autonomic interactions that may be present or for the action of certain antiarrhythmic drugs such as digitalis and adenosine .
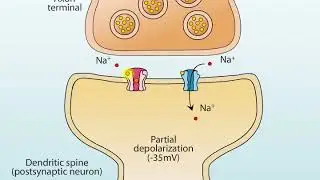
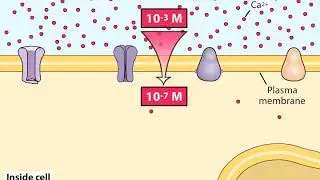
*Class I* — The class I drugs act by modulating or blocking the sodium channels, thereby inhibiting phase 0 depolarization. They are all at least in part positively charged and presumably interact with specific amino acid residues in the internal pore of the sodium channel. Three different subgroups have been identified because their mechanism or duration of action is somewhat different due to variable rates of drug binding to and dissociation from the channel receptor :
●The class IC agents have the slowest binding and dissociation from the receptor.
●The class IB agents have the most rapid binding and dissociation from the receptor.
●The class IA agents are intermediate in terms of the speed of binding and dissociation from the receptor
During faster heart rates, less time exists for the drug to dissociate from the receptor, resulting in an increased number of blocked channels and enhanced blockade. These pharmacologic effects may cause a progressive decrease in impulse conduction velocity and a widening of the QRS complex. This property is known as "use-dependence" and is seen most frequently with the class IC agents, less frequently with the class IA drugs, and rarely with the class IB agents .
●**Class IA drugs (quinidine, procainamide, and disopyramide) depress phase 0 (sodium-dependent) depolarization, thereby slowing conduction. They also have moderate potassium channel blocking activity (which tends to slow the rate of repolarization and prolong action potential duration [APD]), anticholinergic activity, and tend to depress myocardial contractility. At slower heart rates, when use-dependent blockade of the sodium current is not significant, potassium channel blockade may become predominant (reverse use-dependence), leading to prolongation of the APD and QT interval and increased automaticity.
One difference between the drugs is that quinidine and procainamide generally decrease vascular resistance, whereas disopyramide increases vascular resistance. In addition, N-acetyl-procainamide (NAPA), a metabolite of procainamide, has little sodium current blocking activity, while retaining potassium current blocking activity. Thus, NAPA behaves like a class III drug.
●**The class IB drugs (lidocaine and mexiletine) have less prominent sodium channel blocking activity at rest, but effectively block the sodium channel in depolarized tissues. They tend to bind in the inactivated state (which is induced by depolarization) and dissociate from the sodium channel more rapidly than other class I drugs. As a result, they are more effective with tachyarrhythmias than with slow arrhythmias.
●Class IC drugs (flecainide and propafenone) primarily block open sodium channels and slow conduction. They dissociate slowly from the sodium channels during diastole, resulting in increased effect at more rapid rate (use-dependence). This characteristic is the basis for their antiarrhythmic efficacy, especially against supraventricular arrhythmias. Use-dependence may also contribute to the proarrhythmic activity of these drugs, especially in the diseased myocardium, resulting in incessant ventricular tachycardia.
***NO MORE SPACE TO MENTION OTHER 3 CLASSES OF DRUGS****